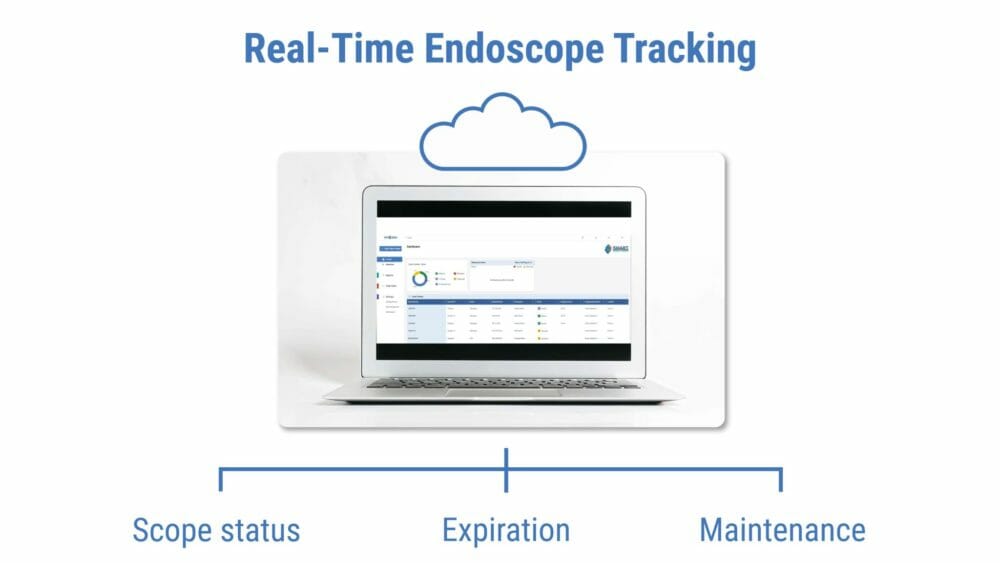
Tracking endoscopes throughout their life cycle is vital to a safe reprocessing program. An electronic tracking system that monitors scope location, disinfection cycles, repairs, maintenance, and real-time status may help identify a scope’s relationship to infectious outbreaks, device recalls, and even trends that may indicate a breakdown in processes.
Scope Reprocessing: An Important Barrier Between Patient and Infectious Organisms
Scope reprocessing begins with pre-cleaning immediately after patient use, followed by a hands-on cleaning and visual inspection to ensure the device is clean and in working order. After sterilization or high-level disinfection, the endoscope must be thoroughly dried and stored in a cabinet that prevents contamination.
Each reprocessing step is critical to reducing the risk of infectious organisms remaining within or on an endoscope. However, even meticulous reprocessing can fail if scopes are improperly dried or stored.
The Association for the Advancement of Medical Instrumentation (AAMI) cited research that explored whether reprocessed endoscopes were safe for patient use. In one study, the number of scopes with residual fluid in the lumens was 95%. In another study, the percentage of endoscopes that retained fluid ranged from almost none to 85%.
If any fluid remains in or on the device, remaining organisms may thrive and multiply, potentially infecting patients.
The drying process is just one area where an electronic scope tracking system can help the facility adhere to its drying and hang times.
Where Are the Scope Reprocessing Recommendations?
Various leading medical societies have published their guidelines for endoscope reprocessing, but there is no clear consensus. Concerns for infectious outbreaks linked to endoscopes have led, in part, to the creation of the Healthcare Infection Control Practices Advisory Committee (HICPAC). HICPAC developed recommendations for flexible endoscope reprocessing after receiving advice from leading medical organizations, including:
- Association for the Advancement of Medical Instrumentation (AAMI);
- American Gastroenterological Association (AGA);
- American Society for Gastrointestinal Endoscopy (ASGE);
- Association of periOperative Registered Nurses (AORN);
- Association for Professionals in Infection Control and Epidemiology (APIC); and
- Centers for Medicare & Medicaid (CMS).
The HICPAC recommendations cover facility set-up, education of staff, developing policies and procedures, reprocessing steps, how to handle a disinfection failure, and documentation.
HICPAC considers documentation and tracking essential to a quality scope reprocessing program. A robust tracking system can assist leadership in responding quickly to a breakdown in processes, an infectious event, or a device recall.
The method of tracking is up to the institution. While paper documentation is permissible, there are significant drawbacks to recording critical data in this manner.
Time pressures and human fallibility can result in incomplete, inaccurate, or illegible documentation. It is challenging to cross-reference data points on a paper log, resulting in missed opportunities to identify issues such as increasing infection rates, skipped processing steps, or expired scopes. And retrieving paper logs during inspections can be time-consuming if the documents are stored outside the endoscopy unit or at a central storage facility.
What Data Should We Track?
An article published in the journal Gastrointestinal Endoscopy Clinics of North America recommends a comprehensive tracking system to aid in tracing infectious outbreaks or quality control issues. Tracking can also ensure consistent maintenance and reprocessing of endoscopes within a facility.
The article’s authors offer endoscope documentation recommendations based on HICPAC’s guidelines, including:
- A unique identifier for each scope;
- Patient identifiers linked to scope use;
- Cleaning times, processes used, maintenance and repair logs;
- An inventory of endoscopes and tracking of all movements, including loans; and
- Identification of any infection control issues with appropriate follow-up.
A comprehensive scope tracking system that is easily searched and cross-referenced can assist in identifying trends. Tracking trends can help managers respond to emerging issues, such as increased infection rates or missed processing steps.
Benefits of an Electronic Scope Drying and Tracking System
Electronic tracking of endoscopes can eliminate the burden of maintaining handwritten logs, alert staff to missed steps during reprocessing, and help managers respond to process failures efficiently and effectively. But tracking shouldn’t end when the reprocessing is complete.
Electronic endoscope storage cabinets can maintain consistent airflow, monitor scope locations, indicate the status of each scope, and display the time left before each scope expires. Monitoring endoscopes in storage can save staff time and reduce the chance that scopes will need to be reprocessed.
Linking endoscope storage units via a cloud-based platform allows managers to monitor inventory, track scope usage, and receive notifications of expired scopes.
The HICPAC endoscopy reprocessing recommendations, developed in consultation with industry leaders, include documentation and tracking of multiple data points. Embracing a robust tracking system that monitors these data points and reduces the risk of overlooking vital steps in reprocessing scopes may lead to better patient outcomes and increased cost savings.